What to Do If You Have a Rash After Scuba Diving

STEVEN P. HUGHES
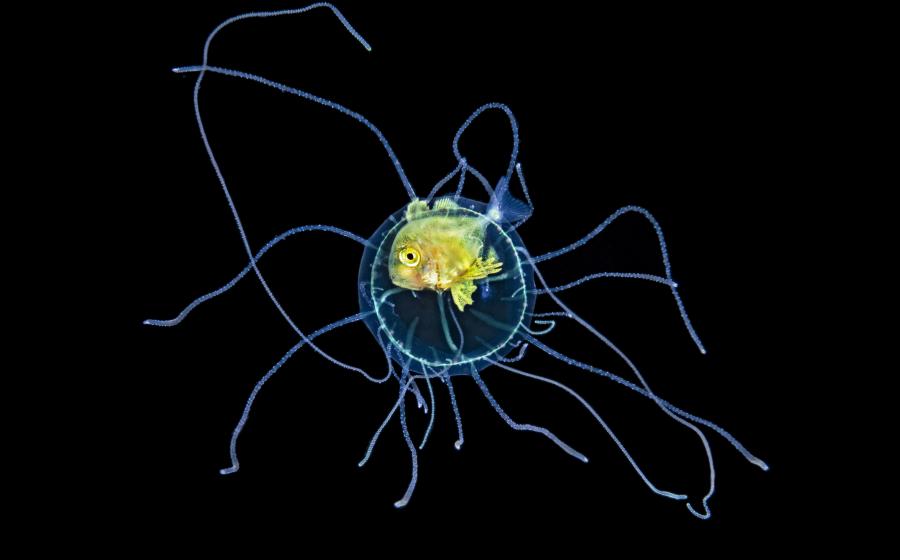
About an hour and a half after her second dive of the day, Jan’s buddy noticed a rash on Jan’s back and hip as she pulled her wetsuit down. They immediately alerted the dive crew.
The Diver
Jan was a 55-year-old diver who learned to dive for her 50th birthday. She made 15 to 20 dives each summer and was in overall good health.
The Dives
Jan and her buddy were on a daylong charter trip with three dives planned. They did two deep dives in the morning to explore an artificial reef. They planned for a shallower dive after a surface interval.
The Accident
After noticing the red and itchy rash on her back and side, Jan removed her wetsuit and took a warm shower. Cortisone cream relieved the itchiness, but her skin remained blotchy.
She called the emergency line at Divers Alert Network (DAN) after consulting with the crew, reporting no other signs or symptoms other than the rash. She had no dizziness, lethargy or loss of her ability to walk normally.
Jan skipped the third dive of the day and went to the emergency room once the boat returned to the dock.
Related Reading: The Risks of Forgoing Drysuit Training
Analysis
A sudden rash while diving could be sea lice or another ocean irritant, but the red-bluish discoloration underneath the skin indicated a likely case of skin bends.
Skin bends is a presentation of decompression sickness (DCS). It is a buildup of nitrogen in the tissues and bloodstream.
When a rash suddenly appears after a dive, especially a deep or long dive, it could signal a bigger issue and requires a full evaluation from a doctor trained in diving medicine. Look for areas of numbness or tingling in the body, extreme tiredness, feeling unsteady on your feet or even problems urinating.
Repeated instances of subcutaneous rashes or other more serious symptoms following diving may be a sign of a patent foramen ovale (PFO)—a hole in the heart wall between the upper chambers of the heart. Under the right conditions, it can allow blood from the venous circulation to pass into the arterial circulation. Nitrogen gas bubbles in the bloodstream would normally be filtered out by the lungs, but when they move into the arterial circulation, they can cause problems. Having a PFO is not a problem in everyday life, but it does increase the risk of more serious neurological DCS symptoms with diving. A surgical procedure can repair it.
Jan’s symptoms continued to resolve as she rested and hydrated. The emergency physician prescribed Benadryl, which seemed to help, but that doesn’t exclude the possibility of skin bends. With a potential DCS case, the boat crew should have administered oxygen.
Some divers make the mistake of diving even after symptoms appear. Jan wisely chose to skip the final dive. She returned to diving a week later but switched to nitrox and dived more conservatively.
Related Reading: What Is Inner Ear Decompression Sickness?
Lessons For Life
Pay attention to your body. When unusual symptoms appear within 24 hours of diving, be aware that you may have a diving-related injury, and consult with DAN.
Understand the signs and symptoms. Learn what to watch for when it comes to decompression sickness.
Learn how to respond. Rescue and oxygen first-aid training prepare you to identify and respond to a suspected case of DCS in your dive buddy or yourself.